Colon & Rectum Cancer
Large intestines; includes the cecum, appendix, ascending and transverse colon, descending and sigmoid colon. The rectum is the last part of the digestive canal and consists of three parts, followed by the anal canal and ends with the anus.

IMAGE: Sections of the Colon
According to the parts of the colon, there are organs with which it is closely adjacent. The part called right hepatic flexure is adjacent to the liver, the duodenum and the gallbladder, while the transverse colon is adjacent to pancreas, stomach and along the lower edge of the liver. Again, the left hepatic flexure has close neighborhoods with the spleen, distal pancreas, and left kidney.
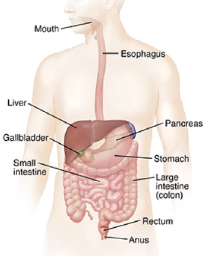
IMAGE: Adjacent Organs to Colon
Colorectal Cancers
Colorectal cancer is a preventable and treatable disease. It is the third most common type of cancer worldwide. Colon and rectal cancers take the second place among cancer-related death rates with 9 percent.
The exact cause of colorectal cancer is unknown, but some known risk factors include; Smoking, alcohol and unhealthy diet carry risks for colon cancer. Considering the factors that increase the risk of colorectal cancer, it is seen that factors such as age, gender, family history, heredity and lifestyle come to the fore. Especially having a family history of colorectal cancer or a history of colorectal polyps is a major risk factor for colon cancer. Another important risk factor is ulcerative colitis and Crohn’s disease, which are inflammatory bowel diseases.
- Being overweight or obese
- Not being physically active
- Excessive consumption of processed food or red meat
- Alcohol Use
- Smoking Cigarette
- Old age
- Having a family history of similar cancer
- Some Genetic Diseases:
- Changes in certain genes increase the risk of colorectal cancer.
- Familial adenomatous polyposis (FAP) is a rare condition characterized by hereditary polyps in the colon and rectum.
- Having had colorectal cancer before: A person with a history of colorectal cancer may develop colorectal cancer again.
- Ulcerative colitis or Crohn’s disease: The risk of colorectal cancer is increased in those with the mentioned inflammatory disease of the intestine.
- Individuals with a first-degree relative with colon cancer have a high incidence of colon cancer.
Most colorectal cancers begin as a growth on the lining of the colon or rectum, which we call polyps. More than 70 percent of colorectal cancers develop from the base of the polyp.

IMAGE : Polyps seen in the colon
It takes about 9 to 12 years for a small polyp to turn into cancer on average. This gives us enough time to remove the polyps. With screening tests, we can prevent 70 percent of deaths due to colorectal cancer. The main purpose of colon cancer screening tests is to prevent the disease, not early diagnosis. Of course, early diagnosis is also a secondary gain, Screening is started with the guaiac fecal occult blood test (gFOBT), and in cases where the test is positive, we have the opportunity to save the patient from the disease and prevent the occurrence of the disease with colonoscopy.
In addition to screening methods, there are some steps to reduce the above risk in the prevention of colon cancers. For example, physical exercise, getting rid of excess weight, not smoking and drinking alcohol, consuming high-fiber, low-fat foods are some of them.

IMAGE: Colonoscopic Polypectomy procedure
Colon rectum cancer Symptoms
The most common symptoms in colorectal cancers are:
- Changes in bowel habits such as diarrhea-constipation and these changes last longer than a few days
- Feeling that you didn’t completely empty your bowels
- Blood in the stool (bright or dark red), or darkening of the stool color
- Abdominal bloating, cramp-like pain or gas complaints
- Weight loss for no known reason
- Constant fatigue
Treatment in colon and rectal cancers
Three main methods are used in the treatment of colorectal cancer: surgery, chemotherapy and radiotherapy. Surgery is the main and most important therapeutic step of colorectal cancer. An operation performed by an experienced surgeon with appropriate technique is the most important form of treatment in colon and rectum cancers. Laparoscopic surgery, robotic surgery and open surgery techniques are used in surgical treatment.
There may be differences in the treatment of colon and rectal cancers. A treatment plan is made according to the region where the cancer is located.
Right hemicolectomy is required if the cancer is in the cecum and ascending colon. The small intestine should then be anastomosed to the transverse colon.
If the tumor is in the transverse colon; The transverse colon is resected and the right colon is anastomosed to the left colon.
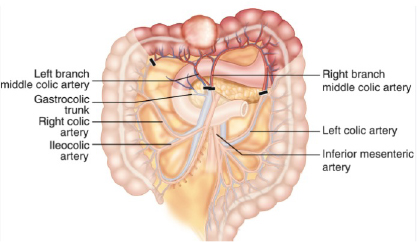
IMAGE: Right Hemicolectomy Surgical Margins
If the tumor is in the descending colon or sigmoid colon, left hemicolectomy is performed and the transverse colon distal is anastomosed to the rectum region.
Tumors in the rectum are evaluated differently from colon tumors. The rectum consists of 3 parts. If a locally advanced stage is detected in preoperative radiological evaluations of a patient diagnosed with cancer, which is valid in all 3 regions of the rectum, chemoradiotherapy may be started first and then surgery may be required. In early stages, the direct decision for surgical treatment is correct. The location of the tumor, its proximity to the anal canal, whether the patient has received neoadjuvant chemoradiotherapy, and some patient-related factors are important for the surgery to be performed. The surgeon should choose the most reliable surgical method for the patient during the operation. In some cases, the small intestine is temporarily attached to the abdominal wall. (Loop Ileostomy)
There are surgical methods such as Anterior Resection, Low Anterior Resection, Ultra Low Anterior Resection for rectal cancers.
For tumors seen in the part which we call the anal canal, chemoradiotherapy may sometimes be required before surgery. There are surgical options according to the evaluations made after these treatments. Sometimes, after the relevant part is removed, anastomosis is performed again, and sometimes the anus is closed by removing the anus and the patient may need to maintain his life with a permanent colostomy. The technique to be applied to the patient should be shared before the surgery and the physician should recommend the most correct one to the patient.
Today, with the development of surgical technologies and the success of experienced surgeons, uncomplicated surgery has developed considerably. Patients who are treated with a suitable surgical method are started to be fed with liquid foods orally on the 2nd day after the operation, and they are discharged 5 days after the operation. When we look at today’s scientific data, it is observed that when the patient’s surgery is performed properly, it goes very well in the postoperative period, but if an operation that does not comply with oncological rules is performed, this situation cannot be resolved with either chemotherapy or radiotherapy. In other words, there is no other treatment that can replace a well-executed surgical treatment. While some of the patients can be completely treated with surgery, others may need treatments such as drugs and chemotherapy.
Get Free Quote